Practice Policies & Patient Information
Access to your Health Records
A request by a patient, or a request by a third party who has been authorised by the patient, for access under the GDPR (and DPA 2018) is called a subject access request (SAR). If you want to see your health records or wish a copy, you can write or call your Practice and then arrange a time to come in and read them. You don’t have to give a reason for wanting to see your records. There is no charge for this service. It’s a good idea to state the dates of the records that you want to see – for example, from 2010-2017 – and to send the letter by recorded delivery or deliver it to the Practice. (if you are requesting this in writing). You should also keep a copy of your letter for your records. The Practice, has up to 28 days to respond. If additional information is needed before copies can be supplied, the 28-day time limit will begin as soon as the additional information has been received. The 28-day time-limit can be extended for two months for complex or numerous requests where the data controller (usually your practice) needs more time to collate and supply the data. You will be informed about this within 28 days and provided with an explanation of why the extension is necessary. When writing/calling, you should say if you: You may also need to fill in an application form and give proof of your identity. The Practice has an obligation under the GDPR and DPA2018 to ensure that any information provided for the patient, can be verified. Please note we never send original medical records because of the potential detriment to patient care should these be lost 1(1) Patients with capacity Subject to the exemptions listed in paragraph 1(6) (below) patients with capacity have a right to access their own health records via a SAR. You may also authorise a third party such as a solicitor to do so on your behalf. Competent young people may also seek access to their own records. It is not necessary for you to give reasons as to why they wish to access their records. 1 (2) Children and young people under 18 Where a child is competent, they are entitled to make or consent to a SAR to access their record. Children aged over 16 years are presumed to be competent. Children under 16 in England, Wales and Northern Ireland must demonstrate that they have sufficient understanding of what is proposed in order to be entitled to make or consent to an SAR. However, children who are aged 12 or over are generally expected to have the competence to give or withhold their consent to the release of information from their health records. In Scotland, anyone aged 12 or over is legally presumed to have such competence. Where, in the view of the appropriate health professional, a child lacks competency to understand the nature of his or her SAR application, the holder of the record is entitled to refuse to comply with the SAR. Where a child is considered capable of making decisions about access to his or her medical record, the consent of the child must be sought before a parent or other third party can be given access via a SAR (see paragraph 1 (3) below) 1(3) Next of kin Despite the widespread use of the phrase ‘next of kin’, this is not defined, nor does it have formal legal status. A next of kin cannot give or withhold their consent to the sharing of information on a patient’s behalf. As next of kin they have no rights of access to medical records. For parental rights of access, see the information above. 1(4) Solicitors You can authorise a solicitor acting on your behalf to make a SAR. We must have your written consent before releasing your medical records to your solicitors acting. The consent must cover the nature and extent of the information to be disclosed under the SAR (for example, past medical history), and who might have access to it as part of the legal proceedings. Where there is any doubt, we may contact you before disclosing the information. (England and Wales only – Should you refuse, your solicitor may apply for a court order requiring disclosure of the information. A standard consent form has been issued by the BMA and the Law Society of England and Wales. While it is not compulsory for solicitors to use the form, it is hoped it will improve the process of seeking consent). The Practice may also contact you to let you know when your medical records are ready. If your solicitor is based within our area, then we may ask you to uplift them and deliver them to your solicitor. This is because we can no longer charge for copying and postage, so we would appreciate your help if you can do this, or alternatively ask your solicitor if they can uplift your medical records. 1(5) Supplementary Information under SAR requests The purpose for which data is processed is for the delivery of healthcare to individual patients. In addition, the data is also processed for other non-direct healthcare purposes such as medical research, public health or health planning purposes when the law allows. The categories of personal data The category of your personal data is healthcare data. The organisations with which the data has been shared Your health records are shared with the appropriate organisations which are involved in the provision of healthcare and treatment to the individual. Other organisations will receive your confidential health information, for example Digital or the Scottish Primary Care Information Resource (SPIRE) or research bodies such as the Secure Anonymised Linkage Databank (SAIL). (This information is already available to patients in our Practice privacy notices). The existence of rights to have inaccurate data corrected and any rights of objection For example, a national ‘opt-out’ model such as SPIRE etc Any automated decision taking including the significance and envisaged consequences for the data subject For example, risk stratification. The right to make a complaint to the Information Commissioner’s Office (ICO) 1(6) Information that should not be disclosed The GDPR and Data Protection Act 2018 provides for a number of exemptions in respect of information falling within the scope of a SAR. If we are unable to disclose information to you, we will inform you and discuss this with you. 1(7)Individuals on behalf of adults who lack capacity Both the Mental Capacity Act in England and Wales and the Adults with Incapacity (Scotland) Act contain powers to nominate individuals to make health and welfare decisions on behalf of incapacitated adults. The Court of Protection in England and Wales, and the Sheriff’s Court in Scotland, can also appoint deputies to do so. This may entail giving access to relevant parts of the incapacitated person’s medical record, unless health professionals can demonstrate that it would not be in the patient’s best interests. These individuals can also be asked to consent to requests for access to records from third parties. Where there are no nominated individuals, requests for access to information relating to incapacitated adults should be granted if it is in the best interests of the patient. In all cases, only information relevant to the purposes for which it is requested should be provided. The law allows you to see records of a patient that has died as long as they were made after 1st November 1991. Records are usually only kept for three years after death (In England and wales GP records are generally retained for 10 years after the patient’s death before they are destroyed). Who can access deceased records? You can only see that person’s records if you are their personal representative, administrator or executor. You won’t be able to see the records of someone who made it clear that they didn’t want other people to see their records after their death. Accessing deceased records Before you get access to these records, you may be asked for: Viewing deceased records You won’t be able to see information that could: 1 (9) To see your hospital records, you will have to contact your local Hospital. 1(10) Your health records are confidential, and members of your family are not allowed to see them, unless you give them written permission, or they have power of attorney. A lasting power of attorney is a legal document that allows you to appoint someone to make decisions for you, should you become incapable of making decisions yourself. The person you appoint is known as your attorney. An attorney can make decisions about your finances, property, and welfare. It is very important that you trust the person you appoint so that they do not abuse their responsibility. A legal power of attorney must be registered with the Office of the Public Guardian before it can be used. If you wish to see the health records of someone who has died, you will have to apply under the Access to Medical Records Act 1990. You can only apply if you: If you think that information in your health records is incorrect, or you need to update your personal details (name, address, phone number), approach the relevant health professional informally and ask to have the record amended. Some hospitals and GP surgeries have online forms for updating your details. If this doesn’t work, you can formally request that the information be amended under the NHS complaints procedure. All NHS trusts, NHS England, CCGs, GPs, dentists, opticians and pharmacists have a complaints procedure. If you want to make a complaint, go to the organisation concerned and ask for a copy of their complaints procedure. Alternatively, you can complain to the Information Commissioner (the person responsible for regulating and enforcing the Data Protection Act), at: The Information Commissioner’s Office (ICO) If your request to have your records amended is refused, the record holder must attach a statement of your views to the record.Subject Access Requests
Who may apply for access?
The purposes for processing data
1(8) Deceased records
Hospital Records
Power of attorney
Wycliffe House
Water Lane
Wilmslow
Cheshire
SK9 5AF
Telephone: 01625 545745
Accessibility
This website is run by your GP Surgery. We want as many people as possible to be able to use this website. For example, that means you should be able to: We’ve also made the website text as simple as possible to understand. AbilityNet has advice on making your device easier to use if you have a disability. We know some parts of this website are not fully accessible: If you need information on this website in a different format please contact We’ll consider your request and get back to you in 30 working days. If you cannot view the map on our ‘contact us’ page, call or email us refer to our contact page for directions. We’re always looking to improve the accessibility of this website. If you find any problems not listed on this page or think we’re not meeting accessibility requirements, contact please contact our practice manager. The Equality and Human Rights Commission (EHRC) is responsible for enforcing the Public Sector Bodies (Websites and Mobile Applications) (No. 2) Accessibility Regulations 2018 (the ‘accessibility regulations’). If you’re not happy with how we respond to your complaint, contact the Equality Advisory and Support Service (EASS). Find out how to contact us on our contact details page. We are committed to making its website accessible, in accordance with the Public Sector Bodies (Websites and Mobile Applications) (No. 2) Accessibility Regulations 2018. This website is partially compliant with the Web Content Accessibility Guidelines version 2.1 AA standard, due to the non-compliances listed below. The content listed below is non-accessible for the following reasons. Some images do not have a text alternative, so people using a screen reader cannot access the information. This fails WCAG 2.1 success criterion 1.1.1 (non-text content). We plan to add text alternatives for all images. When we publish new content we’ll make sure our use of images meets accessibility standards. Some of our interactive forms are difficult to navigate using a keyboard. For example, because some form controls are missing a ‘label’ tag. We’ve assessed the cost of fixing the issues with navigation and accessing information, and with interactive tools and transactions. We believe that doing so now would be a disproportionate burden within the meaning of the accessibility regulations. We will make another assessment when the website is next updated. Many of our older PDFs and Word documents do not meet accessibility standards – for example, they may not be structured so they’re accessible to a screen reader. This does not meet WCAG 2.1 success criterion 4.1.2 (name, role value). Some of our PDFs and Word documents are essential to providing our services. For example, we have PDFs with information on how users can access our services, and forms published as Word documents. We plan to either fix these or replace them with accessible HTML pages. The accessibility regulations do not require us to fix PDFs or other documents published before 23 September 2018 if they’re not essential to providing our services. Any new PDFs or Word documents we publish will meet accessibility standards. Live video streams do not have captions. This fails WCAG 2.1 success criterion 1.2.4 (captions – live). We do not plan to add captions to live video streams because live video is exempt from meeting the accessibility regulations. This website was last tested on October 2019 using the WAV (Web Accessibility Tool) We tested our home page and a random sample of 10 content pages from the site. This statement was prepared on November 2019.
How accessible this website is
What to do if you cannot access parts of this website
Reporting accessibility problems with this website
Enforcement procedure
Contacting us by phone or visiting us in person
Technical information about this website’s accessibility
Non accessible content
Non compliance with the accessibility regulations
Disproportionate burden
Interactive tools and transactions
Content that’s not within the scope of the accessibility regulations
PDFs and other documents
Live video
How we tested this website
Accessible Information Standard
By 31st July 2016 all NHS organisations are required to meet the Accessible Information Standard. This aims to make sure that people with disabilities have access to information that they can understand and any communication support they might need. As part of this process, we want to get better at communicating with our patients. If you find it hard to read our letters or if you need someone to support you at appointments, please let us know. We are keen to hear from you if you have a visual or hearing impairment or another disability and would prefer to receive information in any of the following formats. Please let us know if you, or someone you know has particular communication needs – you may have requirements that are not shown here.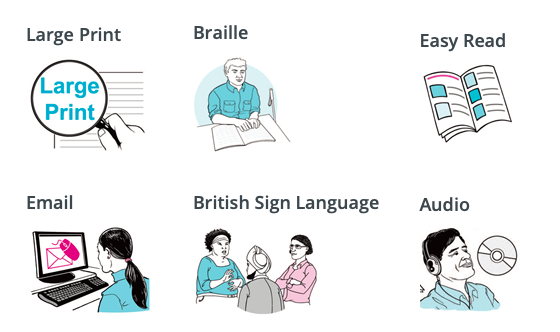
Chaperones
Our Practice is committed to providing a safe, comfortable environment where patient and staff cab be confident that best Practice is being followed at all times and the safety of everyone is of paramount importance. All medical consultations, examinations and investigations are potentially distressing. Patients can find examinations, investigations or photography involving the breasts, genitalia or rectum particularly intrusive (these examinations are collectively referred to as “intimate examinations”). Also consultations involving dimmed lights, the need for patients to undress or for intensive periods of being touched may make a patient feel vulnerable. Chaperoning is the process of having a third person present during such consultations to:- provide support, both emotional and sometimes physical to the patient, and also to protect the doctor against allegations of improper behaviour during such consultations, and sometimes to provide practical support. Please ask clinician , if you want a chaperone.
Clinical Governance
Clinical governance is the system through which NHS organisations are accountable for continuously improving the quality of their services and safeguarding high standards of care by creating an environment in which clinical excellence will flourish Clinical governance encompasses quality assurance, quality improvement and risk and incident management.
Complaints
We make every effort to give the best service possible to everyone who attends our Practice. However, we are aware that things can go wrong resulting in a patient feeling that they have a genuine cause for complaint. If this is so, we would wish for the matter to be settled as quickly, and as amicably, as possible. To have your complaint investigated, you usually need to complain within 12 months of the event happening, or as soon as you first become aware of the issue you want to complain about. The time limit can be extended in special circumstances. If you have a complaint to make, you can either contact the Practice Manager or ask the receptionist for a copy of our complaints Procedure. We endeavour to acknowledge any letter or complaints form within 3 working days of receiving it, and to deal with the matter as promptly as possible- usually within 20 working days- dependent on the nature of the complaint. If the patient’s lack capacity to make decisions, their representative must be able to demonstrate sufficient interest in the patient’s welfare and be an appropriate person to act on their behalf. This could be a partner, relative or someone appointed under the Mental Capacity Act 2005 with lasting power of attorney. In certain circumstances, we need to check that a representative is the appropriate person to make a complaint. If we are not satisfied that the representative is an appropriate person, we cannot consider the complaint, giving the representative reasons for our decision in writing. A complaint must be made within 12 months, either from the date of the incident or from when the complainant first knew about it. The regulations state that a responsible body should consider a complaint after this time limit if: We have a two stage complaints procedure. We will always try to deal with your complaint quickly. However if it is clear that the matter will need a detailed investigation, we will tell you and keep you updated on our progress. If you’re unhappy with the final response from the Practice you can take your complaint to the ombudsman. The ombudsman is independent of the NHS and free to use. It can help resolve your complaint, and tell the NHS how to put things right if it has got them wrong. The ombudsman only has legal powers to investigate certain complaints. You must have received a final response from the Practice before the ombudsman can look at your complaint. The ombudsman will generally not look into your complaint if it happened more than 12 months ago, unless there are exceptional circumstances. Address:In General
Who can complain
Appropriate person
Time limits
Procedure
Stage one – Early, local resolution
Stage Two – Investigation
Complain to the Ombudsman
Parliamentary and Health Service Ombudsman,
Tower, 30
Millbank
London SW1P 4QP
Phone: 0345 015 4033
email
Confidentiality
You have a right to know who holds personal information about you. This person or organisation is called the data controller. In the NHS, the data controller is usually your local NHS board and your GP surgery. The NHS must keep your personal health information confidential. It is your right. Please be aware that our staff are bound to the NHS code of confidentiality. Our staff are therefore not permitted to discuss any of our patient’s medical history, this includes their registration status, without their written consent to do so. Once we have received their written consent and verified this with the patient, then we can provide you with this information, this includes complaining on behalf of a patient, but excludes patients who are unable to act on their own behalf and already have a designated person or carer responsible for their medical care. We therefore respectfully ask parents and guardians not to request information regarding their relatives or to complain on their behalf unless we have their written consent to do so.
Consent Protocol
Consent to treatment is the principle that a person must give permission before they receive any type of medical treatment, test or examination. This must be done on the basis of an explanation by a clinician. Consent from a patient is needed regardless of the procedure, whether it’s a physical examination, organ donation or something else. The principle of consent is an important part of medical ethics and the international human rights law. Defining consent These terms are explained below: If an adult has the capacity to make a voluntary and informed decision to consent to or refuse a particular treatment, their decision must be respected. This is still the case even if refusing treatment would result in their death, or the death of their unborn child. If a person doesn’t have the capacity to make a decision about their treatment, the healthcare professionals treating them can go ahead and give treatment if they believe it’s in the person’s best interests. But clinicians must take reasonable steps to seek advice from the patient’s friends or relatives before making these decisions. Read more about assessing the capacity to consent. How consent is given verbally– for example, by saying they’re happy to have an X-ray in writing– for example, by signing a consent form for surgery Someone could also give non-verbal consent, as long as they understand the treatment or examination about to take place – for example, holding out an arm for a blood test. Consent should be given to the healthcare professional directly responsible for the person’s current treatment, such as: If someone is going to have a major medical procedure, such as an operation, their consent should ideally be secured well in advance, so they have plenty of time to obtain information about the procedure and ask questions. If they change their mind at any point before the procedure, the person is entitled to withdraw their previous consent. Consent from children and young people If they’re able to, consent is usually given by patients themselves. However, someone with parental responsibility may need to give consent for a child up to the age of 16 to have treatment. Read more about the rules of consent applying to children and young people When consent isn’t needed There are a few exceptions when treatment may be able to go ahead without the person’s consent, even if they’re capable of giving their permission. It may not be necessary to obtain consent if a person: requires emergency treatment to save their life, but they’re incapacitated (for example, they’re unconscious) – the reasons why treatment was necessary should be fully explained once they’ve recovered Consent and life-sustaining treatments A person may be being kept alive with supportive treatments – such as lung ventilation – without having made an advance decision, which outlines the care they would refuse to receive. In these cases, a decision about continuing or stopping treatment needs to be made based on what that person’s best interests are believed to be. To help reach a decision, the healthcare professionals responsible for the person’s care should discuss the issue with the relatives and friends of the person receiving the treatment. They should consider, among other things: Treatment can be withdrawn if there’s an agreement that continuing treatment isn’t in the person’s best interests. The case will be referred to the courts before further action is taken if: It’s important to note the difference between withdrawing a person’s life support and taking a deliberate action to make them die. For example, injecting a lethal drug would illegal. Complaints
For consent to be valid, it must be voluntary and informed, and the person consenting must have the capacity to make the decision.
Consent can be given:
is severely ill and living in unhygienic conditions (under the National Assistance Act 1948) – a person who is severely ill or infirm and is living in unsanitary conditions can be taken to a place of care without their consent
If you believe you’ve received treatment you didn’t consent to, you can make an official complaint, please write to the Practice Manager who will assist you with this process.
Duty of Candour
We all share a common purpose as partners in health and social care – and that is to provide high quality care and ensure the best possible outcomes for people using care services. Promoting improvement is at the heart of what we do.We endeavour to provide a first class service at all times. However, we acknowledge that at times things may go wrong and our service may fall below our expected levels.
In order to comply with Regulation 20 of the Health and Social Care Act 2008 (Regulations 2014) we pledge to:
Entitlement to NHS Treatment
The NHS is the UK’s state health service which provides treatment for UK residents. Some services are free, other have to be paid for. The regulations that govern who can and can’t receive treatment are complex and may change. If you are unsure of entitlement to NHS treatment, any charges that may apply, or require further information, please ask the reception staff when you attend the Practice to register, and they will advise you accordingly. GP and nurse consultations in primary care, treatment provided by a GP and other primary care services are free of charge to all, whether registering as an NHS patient, or as a temporary patient, which is when the patient is in the area for more than 24 hours and less than 3 months. For secondary care services, the UK’s healthcare system is a residence-based one, which means entitlement to free healthcare is based on living lawfully in the UK on a properly settled basis for the time being. The measure of residence that the UK uses to determine entitlement to free NHS healthcare is known as ‘ordinary residence’. This requires non-EEA nationals subject to immigration control to also have the immigration status of indefinite leave to remain. Individuals who are not ordinarily resident in the UK may be required to pay for their care when they are in England. However, some services and some individuals are exempt from payment. The following NHS treatment is available to anyone: To qualify for other NHS treatments you must meet certain conditions which are outlined below. Foreign nations from EU member states have reciprocal arrangements for both dental and medical health care so can access the full range of NHS services. Foreign nationals from non-EU countries have no automatic right to NHS healthcare (other than those outlined above). Students and visitors who are going to stay in the UK for less than 6 months would have to be seen as private patients and would have to pay for their treatment. It is therefore essential that you have medical insurance to pay for any Private treatment. If you are not a student registered at a UK university and your are not going to stay in the UK for between six months and a year, it may be unlikely that you will be able receive free NHS Treatment. Be aware that a valid 6 month visa does not automatically confer the right to free NHS treatment. Please note that registering with a GP does not give you automatic entitlement to access free NHS hospital treatment. It is therefore essential that you take out medical insurance for the duration of your visit prior to arrival in the UK. If you are a student registered at a UK University (and you have documentary proof of this) and are going to stay in the UK for more than six months you will qualify for NHS treatment from the beginning of your stay and you (and your dependants) will be entitled to NHS treatment and you may register with a GP. If you need immediate medical assistance (e.g. because of an accident) telephone 999. The call is free. An operator will ask you which emergency service you require (fire, police or ambulance). You will need to tell the emergency services what has happened and where you are. If someone is injured and needs to go to hospital an ambulance will arrive and take them to the nearest hospital with an emergency department. If you need urgent treatment but are well enough to travel please make your own way to the nearest Accident and Emergency Department.Free Services
EU Nationals
Non EU nationals
Medical emergencies
Equality and Diversity
Our policy is designed to ensure and promote equality and inclusion, supporting the ethos and requirements of the Equality Act 2010 for all visitors of our Practice. We are committed to: Procedure Discrimination by the Practice or Visitors / patients against you. If you feel discriminated against: Discrimination against our Practice staff The Practice will not tolerate any form of discrimination or harassment of our staff by any visitor. Any visitor who expresses any form of discrimination against or harassment of any member of our staff will be required to leave the Practice premises immediately. If the visitor is a patient they may also be removed from the Practice list if any such behaviour occurs at the discretion of the Practice Management.
Freedom of Information
Anyone has a right to request information from a public authority. We have two separate duties when responding to these requests: We normally have 20 working days to respond to a request. For a request to be valid under the Freedom of Information Act it must be in writing, Please submit your request to the Practice Manager. Any letter or email to a public authority asking for information is a request for recorded information under the Act.
Infection Control Statement
Infection Prevention and Control is the work an organisation does to identify potential risks for spread of infection between patients (and between patients and staff) and to take measures to reduce that risk. The Practice takes its responsibility to do this very seriously. All staff take responsibility for their own role in this and all staff receive regular training in their role in Infection Prevention and Control.
Named GP Policy
We have allocated a Named Accountable GP for all of our registered patients. New patients joining us will be advised of their Accountable GP ( Dr Bathla) at the point of registration. If you do not know who your named GP is, please ask a member of our reception team.
Privacy Policy
This is the privacy notice of Hockley Medical Practice. In this document, “we”, “our”, or “us” refer to Hockley Medical Practice, 60 Lion Court, Carver Street, Birmingham B1 3AL. Telephone number: 0121 554 1757 Our Practice aims to ensure the highest standard of medical care for our patients. To do this we keep records about you, your health and the care we have provided or plan to provide to you. If you have any questions regarding this privacy policy please contact us at the address shown above. Please view or download our updated data Privacy Notice – November 2021 Please view or download: The law requires us to determine under which of six defined bases we process different categories of your personal information, and to notify you of the basis for each category. If a basis on which we process your personal information is no longer relevant then we shall immediately stop processing your data. If the basis changes then if required by law we shall notify you of the change and of any new basis under which we have determined that we can continue to process your information. When you join our practice, receive medical services from us, or otherwise agree to our terms and conditions, a contract is formed between you and us. In order to carry out our obligations under that contract we must process the information you give us. Some of this information may be personal information. We may use it in order to: We process this information on the basis there is a contract between us, or that you have requested we use the information before we enter into a legal contract. Additionally, we may aggregate this information in a general way and use it to provide class information, for example to monitor our performance with respect to a particular service we provide. If we use it for this purpose, you as an individual will not be personally identifiable. We shall continue to process this information until the contract between us ends or is terminated by either party under the terms of the contract. Through certain actions when otherwise there is no contractual relationship between us, such as when you browse our website or ask us to provide you more information about our business, including job opportunities and our services, you provide your consent to us to process information that may be personal information. Wherever possible, we aim to obtain your explicit consent to process this information, for example, by asking you to agree to our use of cookies. Sometimes you might give your consent implicitly, such as when you send us a message by e-mail to which you would reasonably expect us to reply. Except where you have consented to our use of your information for a specific purpose, we do not use your information in any way that would identify you personally. We may aggregate it in a general way and use it to provide class information, for example to monitor the performance of a particular page on our website. We continue to process your information on this basis until you withdraw your consent or it can be reasonably assumed that your consent no longer exists. You may withdraw your consent at any time by instructing us in writing. However, if you do so, you may not be able to use our website or our services further. We may process information on the basis there is a legitimate interest, either to you or to us, of doing so. Where we process your information on this basis, we do after having given careful consideration to: For example, we may process your data on this basis for the purposes of: We are subject to the law like everyone else. Sometimes, we must process your information in order to comply with a statutory obligation. For example, we may be required to give information to legal authorities if they so request or if they have the proper authorisation such as a search warrant or court order. This may include your personal information. Special category data is personal data which the GDPR says is more sensitive, and so needs more protection. For example information about an individuals: We may process this information for the purposes of medical diagnosis, provision of health treatment and management of health of our patients and the community we serve. Health care professionals who provide you with care maintain records about your health and any treatment or care you have received previously (e.g. NHS Trust, GP Surgery, Walk-in clinic, etc.). These records are used to help to provide you with the best possible healthcare. NHS health care records may be electronic, on paper or a mixture of both, and we use a combination of working practices and technology to ensure that your information is kept confidential and secure. Records this we hold about you may include the following information; To ensure you receive the best possible care, your records are used to facilitate the care you receive. Information held about you may be used to help protect the health of the public and to help us manage the NHS. Information may be used within the GP Practice for clinical audit to monitor the quality of the service provided. Some of this information will be held centrally and used for statistical purposes. Where we do this, we take strict measures to ensure that individual patients cannot be identified. Sometimes your information may be requested to be used for research purposes – the surgery will always gain your consent before releasing the information for this purpose. All staff in the Practice sign a confidentiality agreement that explicitly makes clear their duties in relation to personal health information and the consequences of breaching that duty. Please be aware that your information will be accessed by non-clinical Practice staff in order to perform tasks enabling the functioning of the Practice. These are, but not limited to: The NHS in England uses a national electronic record called the Summary Care Record (SCR) to support patient care. It contains key information from your GP record. Your SCR provides authorised healthcare staff with faster, secure access to essential information about you in an emergency or when you need unplanned care, where such information would otherwise be unavailable. Summary Care Records are there to improve the safety and quality of your care. SCR core information comprises your allergies, adverse reactions and medications. An SCR with additional information can also include reason for medication, vaccinations, significant diagnoses / problems, significant procedures, anticipatory care information and end of life care information. Additional information can only be added to your SCR with your agreement. Please be aware that if you choose to opt-out of SCR, NHS healthcare staff caring for you outside of this surgery may not be aware of your current medications, allergies you suffer from and any bad reactions to medicines you have had, in order to treat you safely in an emergency. Your records will stay as they are now with information being shared by letter, email, fax or phone. If you wish to opt-out of having an SCR please return a completed opt-out formto the practice. ‘Risk stratification for case finding’ is a process for identifying and managing patients who have or may be at-risk of health conditions (such as diabetes) or who are most likely to need healthcare services (such as people with frailty). Risk stratification tools used in the NHS help determine a person’s risk of suffering a particular condition and enable us to focus on preventing ill health before it develops. Further information about risk stratification is available from: https://www.england.nhs.uk/ig/risk-stratification/ If you do not wish information about you to be included in any risk stratification programmes, please let us know. We can add a code to your records that will stop your information from being used for CCG’s and some GP Federations operate pharmacist and prescribing advice services to support local GP practices with prescribing queries, which may require identifiable information to be shared. These pharmacists work with your usual GP to provide advice on medicines and prescribing queries, and review prescribing of medicines to ensure that it is appropriate for your needs, safe and cost-effective. Where specialist prescribing support is required, the CCG medicines management team may order medications on behalf of your GP Practice to support your care. To ensure that adult and children’s safeguarding matters are managed appropriately, access to identifiable information will be shared in some limited circumstances where it’s legally required for the safety of the individuals concerned. Information may be used by the CCG for clinical audit to monitor the quality of the service provided to patients with long terms conditions. Some of this information may be held centrally and used for statistical purposes (e.g. the National Diabetes Audit). When this happens, strict measures are taken to ensure that individual patients cannot be identified from the data. National Registries (such as the Learning Disabilities Register) have statutory permission under Section 251 of the NHS Act 2006, to collect and hold service user identifiable information without the need to seek informed consent from each individual service user. We manage patient records in line with the Records Management NHS Code of Practice for Health and Social Care which sets the required standards of practice in the management of records for those who work within or under contract to NHS organisations in England, based on current legal requirements and professional best practice. If you transfer to another GP and we are asked to transfer your records we will do this to ensure your care is continued. Currently the NHS is required to keep GP records for 10 years after a patient has died. Exceptions to these rules are detailed in the code of practice. If you send us information in connection with a job application, we may keep it for up to three years in case we decide to contact you at a later date. If we employ you, we collect information about you and your work from time to time throughout the period of your employment. This information will be used only for purposes directly relevant to your employment. After your employment has ended, we will keep your file for six years before destroying or deleting it. NHS Digital collects health information from the records health and social care providers keep about the care and treatment they give, to promote health or support improvements in the delivery of care services in England. The NHS Constitution establishes the principles and values of the NHS in England. It sets out the rights patients, the public and staff are entitled to. These rights cover how patients access health services, the quality of care you’ll receive, the treatments and programmes available to you, confidentiality, information and your right to complain if things go wrong. The NHS Care Record Guarantee for England sets out the rules that govern how patient information is used in the NHS, what control the patient can have over this, the rights individuals have to request copies of their data and how data is protected under the Data Protection Act 2018. The use of data by the Cabinet Office for data matching is carried out with statutory authority under Part 6 of the Local Audit and Accountability Act 2014. It does not require the consent of the individuals concerned under the Data Protection Act 2018. Data matching by the Cabinet Office is subject to a Code of Practice. For further information see: National Registries (such as the Learning Disabilities Register) have statutory permission under Section 251 of the NHS Act 2006, to collect and hold service user identifiable information without the need to seek informed consent from each individual service user. An ‘Individual Funding Request’ is a request made on your behalf, with your consent, by a clinician, for funding of specialised healthcare which falls outside the range of services and treatments that CCG has agreed to commission for the local population. An Individual Funding Request is taken under consideration when a case can be set out by a patient’s clinician that there are exceptional clinical circumstances which make the patient’s case different from other patients with the same condition who are at the same stage of their disease, or when the request is for a treatment that is regarded as new or experimental and where there are no other similar patients who would benefit from this treatment. A detailed response, including the criteria considered in arriving at the decision, will be provided to the patient’s clinician. Invoice validation is an important process. It involves using your NHS number to check which CCG is responsible for paying for your treatment. Section 251 of the NHS Act 2006 provides a statutory legal basis to process data for invoice validation purposes. We can also use your NHS number to check whether your care has been funded through specialist commissioning, which NHS England will pay for. The process makes sure that the organisations providing your care are paid correctly. When you contact us, whether by telephone, through our website or by e-mail, we collect the data you have given to us in order to reply with the information you need. We record your request and our reply in order to increase the efficiency of our Practice. We keep personally identifiable information associated with your message, such as your name and email address so as to be able to track our communications with you to provide a high quality service. When we receive a complaint, we record all the information you have given to us. We use that information to resolve your complaint. If your complaint reasonably requires us to contact some other person, we may decide to give to that other person some of the information contained in your complaint. We do this as infrequently as possible, but it is a matter for our sole discretion as to whether we do give information, and if we do, what that information is. We may also compile statistics showing information obtained from this source to assess the level of service we provide, but not in a way that could identify you or any other person. Cookies are small text files that are placed on your computer’s hard drive by your web browser when you visit any website. They allow information gathered on one web page to be stored until it is needed for use on another, allowing a website to provide you with a personalised experience and the website owner with statistics about how you use the website so that it can be improved. Some cookies may last for a defined period of time, such as one day or until you close your browser. Others last indefinitely. Your web browser should allow you to delete any you choose. It also should allow you to prevent or limit their use. Our website uses cookies. They are placed by software that operates on our servers, and by software operated by third parties whose services we use. If you choose not to use cookies or you prevent their use through your browser settings, you will not be able to use all the functionality of our website. We use cookies in the following ways: Requests by your web browser to our servers for web pages and other content on our website are recorded. We record information such as your geographical location, your Internet service provider and your IP address. We also record information about the software you are using to browse our website, such as the type of computer or device and the screen resolution. We use this information in aggregate to assess the popularity of the webpages on our website and how we perform in providing content to you. If combined with other information we know about you from previous visits, the data possibly could be used to identify you personally, even if you are not signed in to our website. We sometimes receive data that is indirectly made up from your personal information from third parties whose services we use. No such information is personally identifiable to you. We will only ever use or pass on information about you if others involved in your care have a genuine need for it. We will not disclose your information to any third party without your permission unless there are exceptional circumstances (i.e. life or death situations), where the law requires information to be passed on and / or in accordance with the new information sharing principle following Dame Fiona Caldicott’s information sharing review (Information to share or not to share) where “The duty to share information can be as important as the duty to protect patient confidentiality.”This means that health and social care professionals should have the confidence to share information in the best interests of their patients within the framework set out by the Caldicott principles. They should be supported by the policies of their employers, regulators and professional bodies. We may also have to share your information, subject to strict agreements on how it will be used, with the following organisations; You will be informed who your data will be shared with and in some cases asked for explicit consent for this happen when this is required. We may also use external companies to process personal information, such as for archiving purposes. These companies are bound by contractual agreements to ensure information is kept confidential and secure. Our website is hosted in the United Kingdom. We may also use outsourced services in countries outside the European Union from time to time in other aspects of our business. Accordingly data obtained within the UK or any other country could be processed outside the European Union. For example online patient forms on our website are encrypted and delivered securely to the NHS system by an email service provider based in the United States of America. Their systems comply with provisions certified under the EU-U.S. and Swiss-U.S. Privacy Shield frameworks, a mechanism for cross border transfer of personal data. If you wish us to remove personally identifiable information from our website, please get in touch. This may limit the service we can provide to you. When we receive any request to access, edit or delete personal identifiable information we shall first take reasonable steps to verify your identity before granting you access or otherwise taking any action. This is important to safeguard your information. Your GP electronic patient record is held securely and confidentially on an electronic system managed by your registered GP practice. If you require attention from a local health or care professional outside of your usual practice services, such as in an Evening and Weekend GP Access Clinic, GP Federation Service, Emergency Department, Minor Injury Unit or Out Of Hours service, the professionals treating you are better able to give you safe and effective care if some of the information from your GP record is available to them. Where available, this information can be shared electronically with other local healthcare providers via a secure system designed for this purpose. Depending on the service you are using and your health needs, this may involve the healthcare professional accessing a secure system that enables them to view parts of your GP electronic patient record ,or a secure system that enables them to view your full GP electronic patient record (e.g. EMIS remote consulting system). In all cases, your information is only accessed and used by authorised staff who are involved in providing or supporting your direct care. Your permission will be asked before the information is accessed, other than in exceptional circumstances (e.g. emergencies) if the healthcare professional is unable to ask you and this is deemed to be in your best interests (which will then be logged). We use Secure Sockets Layer (SSL) certificates to verify our identity to your browser and to encrypt any data you give us. Whenever information is transferred between us, you can check that it is done so using SSL by looking for a closed padlock symbol or other trust mark in your browser’s URL bar or toolbar. If you are happy for your data to be extracted and used for the purposes described in this privacy notice then you do not need to do anything. If you have any concerns about how your data is shared then please contact the Practice. The Practice Data Protection Officer is: Judith Jordon, Contact address: NHS Arden and Greater East Midlands Commissioning Support Unit Westgate House Market Street, Warwick CV34 4DE Telephone: 0121 611 0730 or Email: agem.dpo@nhs.net The Data Protection Act 2018 requires organisations to register a notification with the Information Commissioner to describe the purposes for which they process personal and sensitive information. Our practice is legally required to provide anonymised data on patients who have been issued with a fit note under the Fit for Work scheme. The purpose is to provide the Department for Work and Pensions with information from fit notes to improve the monitoring of public health and commissioning and quality of health services. It is important that you tell the person treating you if any of your details such as your name or address have changed or if any of your details such as date of birth is incorrect in order for this to be amended. You have a responsibility to inform us of any changes so our records are accurate and up to date for you. You have a right to object to your information being shared. Should you wish to opt out of data collection, please contact a member of staff who will be able to explain how you can opt out and prevent the sharing of your information; this is done by registering a Type 1 opt-out, preventing your information from being shared outside this Practice. If you have previously opted-out of any data sharing arrangements, your opt-out I will continue to be valid. Our privacy policy has been compiled so as to comply with the law of every country or legal jurisdiction in which we aim to do business. If you think it fails to satisfy the law of your jurisdiction, we should like to hear from you. However, ultimately it is your choice as to whether you wish to use our website. It is important to point out that we may amend this Privacy Notice from time to time. If you are dissatisfied with any aspect of our Privacy Notice, please contact the Practice Data Protection Officer.Introduction
Data Privacy Notice
Candidate Privacy Notice
The bases on which we process information about you
Information we process because we have a contractual obligation with you
Information we process with your consent
Information we process for the purposes of legitimate interests
Information we process because we have a legal obligation
Information we process may be categorised as special category data
Specific uses of information you provide to us
Who Else May Ask to Access Your Information
Anyone Who Receives Information From us is Also Under a Legal Duty to Keep it Confidential and Secure
Summary Care Record (SCR)
Risk Stratification
Information about you is collected from a number of sources including NHS Trusts, GP Federations and your GP Practice. A risk score is then arrived at through an analysis of your de-identified information. This can help us identify and offer you additional services to improve your health. Risk-stratification data may also be used to improve local services and commission new services, where there is an identified need. In this area, risk stratification may be commissioned by the our NHS Clinical Commissioning Group (OCCG). Section 251 of the NHS Act 2006 provides a statutory legal basis to process data for risk stratification purposes.
this purpose. Please be aware that this may limit the ability of healthcare professionals to identify if you have or are at risk of developing certain serious health conditions.Medicines Management
Supporting Locally Commissioned Services CCGs support GP practices by auditing anonymised data to monitor locally commissioned services, measure prevalence and support data quality. The data does not include identifiable information and is used to support patient care and ensure providers are correctly paid for the services they provide.Safeguarding
Clinical audit
National Registries
Data Retention
Job application and employment
NHS Digital
http://content.digital.nhs.uk/article/4963/What-we-collectThe NHS Constitution
https://www.gov.uk/government/publications/the-nhs-constitution-for-englandThe NHS Care Record Guarantee
https://digital.nhs.uk/data-and-information/looking-after-information/data-security-and-information-governanceNational Fraud Initiative – Cabinet Office
https://www.gov.uk/government/publications/code-of-data-matching-practice-for-national-fraud-initiativeNational Registries
Individual Funding Request
Invoice Validation
Sending a message to our Practice team
Complaining
Use of information we collect through automated systems when you visit our website
Cookies
Personal identifiers from your browsing activity
Disclosure and sharing of your information
Information we obtain from third parties
Information provided on the understanding that it will be shared with a third party
Who are our partner organisations?
Data may be processed outside the European Union
Access to your own information
Access to your personal information
Removal of your information
Verification of your information
Local Information Sharing
Other matters
Use of our website by children
Encryption of data sent between us
How you can complain
Wycliffe House
Water Lane
Wilmslow
Cheshire
SK9 5AF
Phone: 0303 123 1113Data Protection Officer
Associate Director Of Integrated GovernanceNotification
We are registered as a data controller and our registration can be viewed online in the public register at: http://ico.org.uk/what_we_cover/register_of_data_controllers
Any changes to this notice will be published on our website and in a prominent area at the Practice.Department for Work and Pensions
Change of Details
Opt-outs
Compliance with the law
Review of this privacy policy
Quality Assurance
Our practice aims to provide primary care of a consistent quality for all patients. We strive to meet the high standards expected in any clinical setting. We expect all our members of our team to work to these standards to help us achieve our aim of providing a quality service. The policies, systems and processes in place in your Practice reflect our professional and legal responsibilities and follow recognised standards of good Practice. We evaluate our Practice on a regular basis, through audit, peer review and patient feedback and monitor the effectiveness of our quality assurance procedures. In providing our patients with care of a consistent quality we will: In providing our team with care of a consistent quality we will:Quality standards and procedures
Removal of Patients From our List
It is our policy not to remove patients without serious consideration. If a patient has a serious continuing medical condition, removal will be postponed until the patient’s condition stabilises. Possible grounds for consideration of removal include: It should be noted that if a patient does not attend for their appointment they will not be given another one for 48 hours. In the event of a patient not attending on three occasions they will receive a letter advising them that if they miss another appointment they will be removed from our Practice list. In some cases we reserve the right to remove other members of the household. We will continue to be responsible for the patient’s medical care for a period of up to 8 days from the date of notification to our local health authority or until the patient registers with another doctor, whichever is the sooner.
Safeguarding Children
Our primary care team is committed to safeguarding children across the organisation. The safety and welfare of children who come into contact with our services either directly or indirectly is paramount and all staff have a responsibility to ensure that best Practice is followed, including compliance with statutory requirements. We are committed to a best Practice which safeguards children and young people irrespective of their background, and which recognises that a child may be abused regardless of their age, gender, religious beliefs, racial origin or ethnic identity, culture, class, disability or sexual orientation. The primary care team are committed to working within agreed policies and procedures and in partnership with other agencies to ensure that the risks of harm to a child or young person are minimised. This work may include direct and indirect contact with children, (access to patient’s details, communication via email, text message/phone). Our organisation is being supported by the CCG who have Designated Nurses and Doctors in post to offer professional expertise and advice regarding safeguarding matters.
Sharing your Information with Others
Collecting and sharing information is essential to provide safe and effective health care. Appropriate information sharing is an essential part of the provision of safe and effective care. Patients may be put at risk if those who provide their care do not have access to relevant, accurate and up-to-date information about them. All staff have an ethical and legal duty to keep patient information confidential. If you do not wish your health information shared please notify the Practice in writing, so we may update your record.
Summary Care Records (SCR)
Summary Care Records (SCR) are an electronic record of important patient information, created from GP medical records. It can be seen and used by authorised staff in other areas of the health and care system involved in the patient’s direct care. Your Summary Care Record Care professionals in England use an electronic record called the Summary Care Record (SCR). This can provide those involved in your care with faster secure access to key information from your GP record. If you are registered with a GP Practice in England, you will already have an SCR unless you have previously chosen not to have one. It includes the following basic information: It also includes your name, address, date of birth and unique NHS Number which helps to identify you correctly. You can now choose to include more information in your SCR, such as significant medical history (past and present), information about management of long term conditions, immunisations and patient preferences such as end of life care information, particular care needs and communication preferences. If you would like to do this, talk to your GP Practice as it can only be added with your permission. Remember, you can change your mind about your SCR at any time. Talk to your GP Practice if you want to discuss your option to add more information or decide you no longer want an SCR. Having an SCR that includes extra information can be of particular benefit to patients with detailed and complex health problems. If you are a carer for someone and believe that this may benefit them, you could discuss it with them and their GP Practice. Only authorised care professional staff in England who are involved in your direct care can have access to your SCR. Your SCR will not be used for any other purposes. These staff: Care professionals will ask for your permission if they need to look at your SCR. If they cannot ask you because you are unconscious or otherwise unable to communicate, they may decide to look at your record because doing so is in your best interest. This access is recorded and checked to ensure that it is appropriate. If you are the parent or guardian of a child under 16, and feel they are able to understand this information you should show it to them. You can then support them to come to a decision about having an SCR and whether to include additional information. For information on how the NHS will collect, store and allow access to your electronic records visit NHS Choices.What is a SCR?
What choices do you have?
Vulnerable patients and carers
Who can see my SCR?
SCRs for children
Confidentiality
Unacceptable Actions Policy
We believe that patients have a right to be heard, understood and respected. We work hard to be open and accessible to everyone. Occasionally, the behaviour or actions of individuals using our Practice makes it very difficult for us to deal with their issue or complaint. In a small number of cases the actions of individuals become unacceptable because they involve abuse of our staff or our process. When this happens we have to take action to protect our staff. We also consider the impact of the behaviour on our ability to do our work and provide a service to others. This Policy explains how we will approach these situations. People may act out of character in times of trouble or distress. There may have been upsetting or distressing circumstances leading up to us being made aware of an issue or complaint. We do not view behaviour as unacceptable just because a patient is forceful or determined. In fact, we accept that being persistent may sometimes be a positive advantage when pursuing an issue or complaint. However, we do consider actions that result in unreasonable demands on our Practice or unreasonable behaviour towards Practice staff to be unacceptable. It is these actions that we aim to manage under this Policy. We understand that patients may be angry about the issues they have raised with the Practice. If that anger escalates into aggression towards Practice staff, we consider that unacceptable. Any violence or abuse towards staff will not be accepted. Violence is not restricted to acts of aggression that may result in physical harm. It also includes behaviour or language (whether verbal or written) that may cause staff to feel offended, afraid, threatened or abused. We will judge each situation individually and appreciate individuals who come to us may be upset. Language which is designed to insult or degrade, is derogatory, racist, sexist, transphobic, or homophobic or which makes serious allegations that individuals have committed criminal, corrupt, perverse or unprofessional conduct of any kind, without any evidence, is unacceptable. We may decide that comments aimed not at us, but at third parties, are unacceptable because of the effect that listening or reading them may have on our staff. A demand becomes unacceptable when it starts to (or when complying with the demand would) impact substantially on the work of the Practice. Examples of actions grouped under this heading include: Sometimes the volume and duration of contact made to our Practice by an individual causes problems. This can occur over a short period, for example, a number of calls in one day or one hour. It may occur over the life-span of an issue when a patient repeatedly makes long telephone calls to us, or inundates us with letters or copies of information that have been sent already or that are irrelevant to the issue. We consider that the level of contact has become unacceptable when the amount of time spent talking to a patient on the telephone, or responding to, reviewing and filing emails or written correspondence impacts on our ability to deal with that issue, or with other Patients’ needs. When we are looking at an issue or complaint, we will ask the patient to work with us. This can include agreeing with us the issues or complaint we will look at; providing us with Sometimes, a patient repeatedly refuses to cooperate and this makes it difficult for us to proceed. We will always seek to assist someone if they have a specific, genuine difficulty complying with a request. However, we consider it is unreasonable to bring an issue to us and then not respond to reasonable requests. Individuals with complaints about the Practice have the right to pursue their concerns through a range of means. They also have the right to complain more than once about the Practice, if subsequent incidents occur. This contact becomes unreasonable when the effect of the repeated complaints is to harass, or to prevent us from pursuing a legitimate aim or implementing a legitimate decision. We consider access to a complaints system to be important and it will only be in exceptional circumstances that we would consider such repeated use is unacceptable – but we reserve the right to do so in such cases. We have to take action when unreasonable behaviour impairs the functioning of our Practice. We aim to do this in a way that allows a Patient to progress through our process. We will try to ensure that any action we take is the minimum required to solve the problem, taking into account relevant personal circumstances including the seriousness of the issue(s) or complaint and the needs of the individual. Where a patient repeatedly phones, visits the Practice, raises repeated issues, or sends largenumbers of documents where their relevance isn’t clear, we may decide to: • limit contact to telephone calls from the patient about the issues raised at set times on set days • restrict contact to a nominated member of the Practice staff who will deal with future calls or correspondence from the patient about their issues • see the patient by appointment only • restrict contact from the patient to writing only regarding the issues raised. • return any documents to the patient or, in extreme cases, advise the patient that further irrelevant documents will be destroyed. • take any other action that we consider appropriate. Where we consider continued correspondence on a wide range of issues to be excessive, we may tell the patient that only a certain number of issues will be considered in a given period and we ask them to limit or focus their requests accordingly. In exceptional cases, we reserve the right to refuse to consider an issue, or future issues or complaints from an individual. We will take into account the impact on the individual and also whether there would be a broader public interest in considering the issue or complaint further. We will always tell the patient what action we are taking and why. When a Practice employee makes an immediate decision in response to offensive, aggressive or abusive behaviour, the patient is advised at the time of the incident. When a decision has been made by Senior Management, a patient will always be given the reason in writing as to why a decision has been made to issue a warning (including the We record all incidents of unacceptable actions by patients. Where it is decided to issue a warning to a patient, an entry noting this is made in the relevant file and on appropriate computer records. Each quarter a report on all restrictions will be presented to our Senior Management Team so that they can ensure the policy is being applied appropriately. A decision to issue a warning to a patient as described above may be reconsidered either on request or on review. It is important that a decision can be reconsidered. A patient can appeal a decision about the issuance of a warning or removal from the Practice list. If they do this, we will only consider arguments that relate to the warning or removal, and not to either the issue or complaint made to us, or to our decision to close a complaint. An appeal could include, for example, a patient saying that: their actions were wrongly identified as unacceptable; the warning was disproportionate; or that it will adversely impact on the individual because of personal circumstances. The Practice Manager or a GP Partner who was not involved in the original decision will consider the appeal. They have discretion to quash or vary the warning as they think best. They will make their decision based on the evidence available to them. They must advise the patient in writing that either the warning or removal still applies or a different course of action has been agreed. We may review the warning periodically or on further request after a period of time has passed. Each case is different. This policy is subject to reviewSection 1 – What actions does the Practice consider to be unacceptable?
Section 2 – Aggressive or abusive behaviour
Section 3 – Unreasonable demands
Section 4 – Unreasonable levels of contact
Section 5 – Unreasonable refusal to co-operate
further information, evidence or comments on request; or helping us by summarising their concerns or completing a form for us.Section 6 – Unreasonable use of the complaints process
Section 7 – Examples of how we manage aggressive or abusive behaviour
Section 8 – Examples of how we deal with other categories of unreasonable behaviour
Section 9 – Other actions we may take
Section 10 – The process we follow to make decisions about unreasonable behaviour
Section 11 – How we let people know we have made this decision
duration and terms of the warning) or remove them from the Practice list. This ensures that the patient has a record of the decision.Section 12 – How we record and review a decision to issue a warning
Section 13 – The process for appealing a decision
Zero Tolerance
The Practice will not tolerate violent or abusive behaviour. Anyone verbally abusing either a member of staff or the public, or using inappropriate language, will be asked to leave the premises and requested to find another GP. Anyone who is violent or causes damage will be removed from the list immediately. Patients will also be removed from the list in the following circumstances: Patients who are disruptive and display aggressive and/or intimidating behaviour and refuse to leave the premises, staff are instructed to dial 999 for Police assistance, charges may then be brought against these individuals.